Fill in a Valid Tb Test Form
Common PDF Forms
What Countries Require International Driving Permit - Applicants should keep copies of their submitted forms for their records.
When navigating the complexities of property transactions, understanding the key elements of the Real Estate Purchase Agreement is crucial for both buyers and sellers. To familiarize yourself with this important document, consider exploring a resource that provides insightful tips and guidelines for creating your own real estate purchase agreement. Visit comprehensive insights into the Real Estate Purchase Agreement to get started.
T47 Affidavit - Completing the T-47 can facilitate a smoother closing process for buyers and lenders.
Advance Salary Application Form - This form is a straightforward way to address pressing needs prior to receiving your paycheck.
Misconceptions
Understanding the Tuberculosis (TB) test form is crucial for both healthcare professionals and patients. However, several misconceptions can lead to confusion regarding its purpose and use. Below is a list of common misconceptions about the TB test form, along with clarifications.
- The TB test form is only for patients who show symptoms of TB. In reality, the form is used for anyone being tested for TB, regardless of symptoms.
- Only doctors can administer the TB test. Nurses and other qualified healthcare professionals can also administer the test and sign the form.
- The results of the TB test are immediate. The results must be read 48-72 hours after the test is administered, which is why the form includes a section for the date read.
- A negative result means no exposure to TB. A negative result indicates no current infection, but it does not guarantee that a person has never been exposed to the bacteria.
- Positive results always indicate active TB disease. A positive result may indicate latent TB infection, which does not show symptoms but requires monitoring and possible treatment.
- The expiration date on the form is irrelevant. The expiration date of the PPD (purified protein derivative) must be observed, as using expired materials can yield inaccurate results.
- Completion of the form is optional. All sections of the TB test form must be completed for it to be valid and acceptable.
- Only one signature is required on the form. The form requires signatures from both the person administering the test and the individual reading the results.
- Induration measurement is not important. The size of the induration, measured in millimeters, is critical for interpreting the test results accurately.
By addressing these misconceptions, patients and healthcare providers can ensure proper understanding and handling of the TB test process.
Documents used along the form
When dealing with tuberculosis testing, several other forms and documents may be necessary to ensure comprehensive health management. Each of these documents plays a role in tracking patient information, results, and follow-up actions. Below is a list of common forms that are often used alongside the TB Test form.
- Patient Health History Form: This document gathers essential information about the patient’s medical history, including previous illnesses, allergies, and current medications. It helps healthcare providers assess the patient's risk factors for tuberculosis.
- Consent Form: Patients must sign this form to give permission for the TB test to be conducted. It outlines the procedure, potential risks, and the patient's right to withdraw consent at any time.
- Motor Vehicle Bill of Sale Form: For accurate vehicle ownership transfers, leverage our essential Motor Vehicle Bill of Sale form guidelines to ensure all legal requirements are met.
- Follow-Up Evaluation Form: After the TB test results are obtained, this form is used to document any necessary follow-up actions. It may include recommendations for further testing or treatment based on the results.
- Referral Form: If the TB test result is positive, a referral form may be used to direct the patient to a specialist for further evaluation and treatment. This ensures that the patient receives the appropriate care.
- Immunization Record: This document tracks the patient’s vaccination history, which can be important in understanding their overall health status and any potential exposure to tuberculosis.
Having these documents in order can help streamline the testing process and provide better care for patients. Each form serves a specific purpose and contributes to a thorough understanding of the patient’s health regarding tuberculosis.
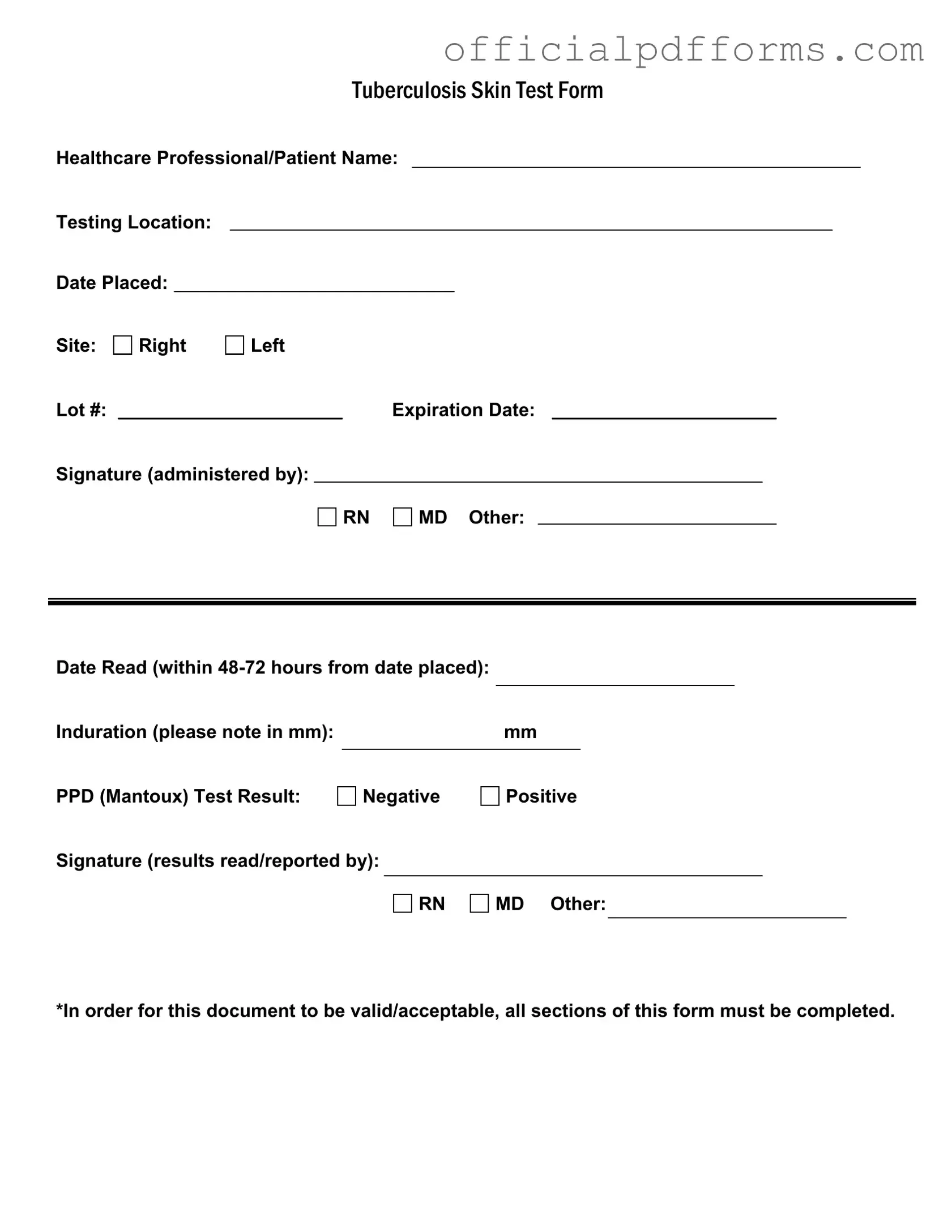
Steps to Filling Out Tb Test
After you receive the Tb Test form, you'll need to fill it out completely to ensure it is valid. This form collects essential information about the test and its administration. Make sure to provide accurate details in each section.
- Start by entering the name of the healthcare professional and the patient at the top of the form.
- Next, fill in the testing location where the test is being administered.
- Record the date the test was placed.
- Indicate the site of the test, specifying whether it was on the right or left arm.
- Write down the lot number of the test.
- Provide the expiration date of the test.
- The healthcare professional administering the test should sign in the designated area.
- Note the date when the test results will be read, ensuring it falls within 48-72 hours from the date placed.
- Measure the induration in millimeters and write that number in the specified space.
- Mark the result of the PPD (Mantoux) test as either negative or positive.
- Finally, the healthcare professional who reads the results must sign the form, indicating their title (RN, MD, or other).
Once you have completed all these steps, review the form to ensure all sections are filled out correctly. This will help prevent any issues with the validity of the document.
Common mistakes
-
Failing to fill in the healthcare professional's name clearly. This can lead to confusion about who administered the test.
-
Not specifying the testing location. Without this information, tracking the test becomes difficult.
-
Leaving the date placed section blank. This date is crucial for determining when the test results should be read.
-
Neglecting to indicate the site of the test. Indicating whether it was done on the right or left arm is essential.
-
Not including the lot number. This information is necessary for quality control and traceability.
-
Forgetting to write the expiration date of the test materials. Using expired materials can lead to inaccurate results.
-
Not signing the form where it states signature (administered by). This signature confirms who performed the test.
-
Overlooking the date read section. Results must be read within 48-72 hours, and this date must be recorded.
-
Failing to note the induration measurement in millimeters. This measurement is critical for interpreting the results.
-
Not marking the PPD test result as negative or positive. This is the most important part of the form and must be clear.
Get Clarifications on Tb Test
What is the purpose of the TB Test form?
The TB Test form is used to document the administration and results of the Tuberculosis (TB) skin test, also known as the PPD (Purified Protein Derivative) test. This form serves as an official record for healthcare providers and patients, ensuring that all necessary information is captured for accurate evaluation of TB exposure.
Who can administer the TB Test?
The TB Test can be administered by qualified healthcare professionals, including Registered Nurses (RNs) and Medical Doctors (MDs). The form requires the signature of the person who administered the test to validate the procedure.
What information is required on the TB Test form?
To ensure the form is valid, all sections must be completed. Required information includes:
- Healthcare Professional/Patient Name
- Testing Location
- Date Placed
- Site of administration (Right or Left arm)
- Lot number and expiration date of the PPD
- Signature of the administering professional
- Date Read (within 48-72 hours)
- Induration measurement in mm
- Test result (Negative or Positive)
- Signature of the professional who read the results
How soon should the test results be read?
The results of the TB skin test should be read within 48 to 72 hours after the test is administered. It is crucial to adhere to this time frame to ensure accurate interpretation of the induration measurement.
What does the induration measurement indicate?
Induration refers to the raised, hardened area at the site of the TB test. The measurement is taken in millimeters (mm) and is used to determine the test result. A larger induration may indicate a positive reaction, suggesting potential exposure to TB. However, the interpretation can vary based on individual risk factors.
What does a positive TB test result mean?
A positive TB test result indicates that the individual has been exposed to the bacteria that cause tuberculosis. This does not necessarily mean the person has active TB disease. Further evaluation, including a chest X-ray or additional tests, may be required to determine if the infection is latent or active.
What should I do if my test result is negative?
A negative TB test result generally indicates that there has been no exposure to the TB bacteria. However, if you have symptoms of TB or have been in close contact with someone who has active TB, consult your healthcare provider for further assessment and possible follow-up testing.
Is there a need for follow-up testing?
Follow-up testing may be necessary depending on the initial test results and individual risk factors. If the test is positive, further diagnostic procedures will be needed. For individuals at high risk or with previous positive results, periodic testing may also be recommended. Always discuss your specific situation with a healthcare professional.