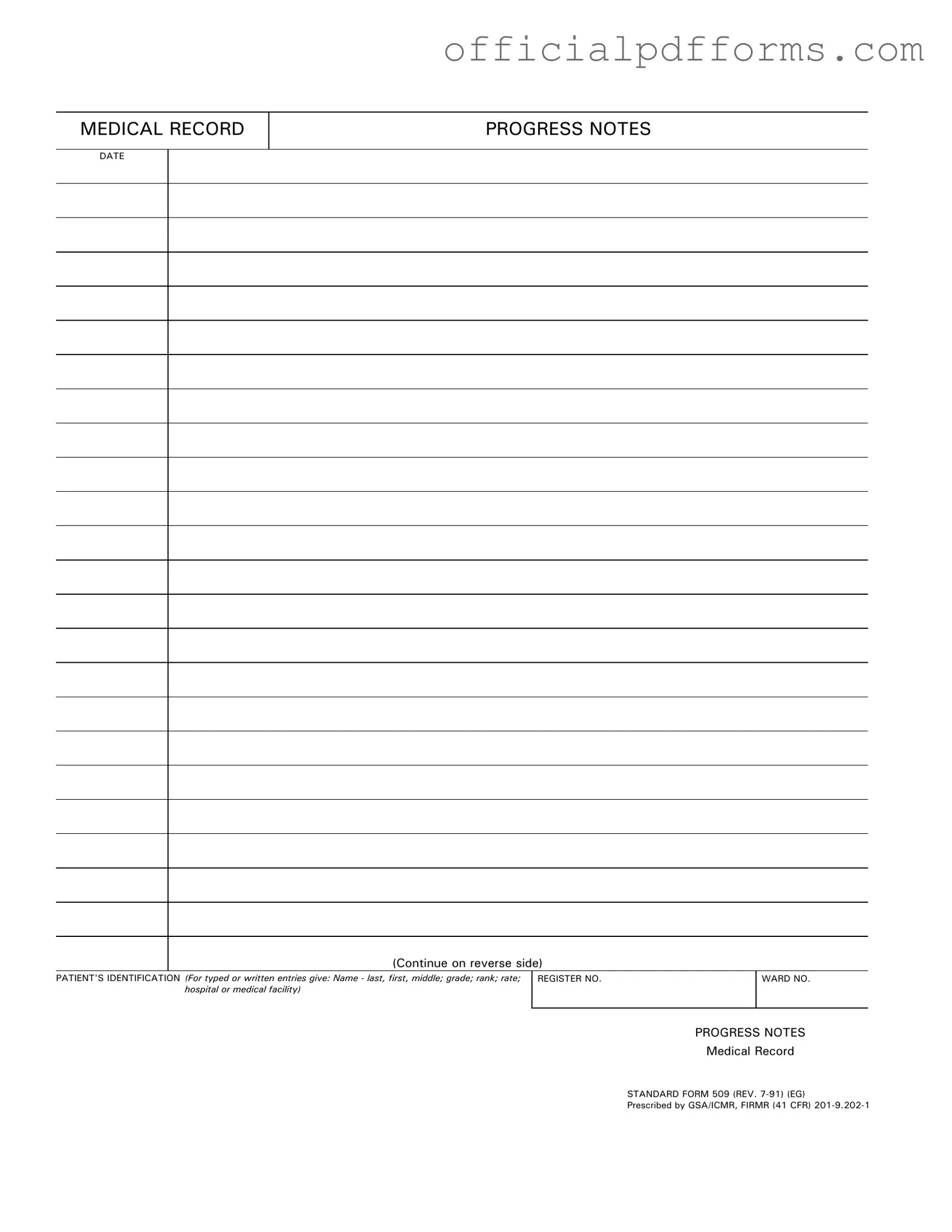
Fill in a Valid Progress Notes Form
Common PDF Forms
Dd Form 2870 Army Pubs - The form aids in organizing a patient’s medical documentation for review.
Understanding the importance of the Sample Tax Return Transcript form is crucial for individuals navigating tax-related processes, as it can be beneficial for verifying income during loan applications or financial assessments. For more detailed insights into obtaining and utilizing this document, consider visiting OnlineLawDocs.com.
Home Load Calculation - Detailing both continuous and non-continuous loads is a key aspect of this form.
Misconceptions
Misconceptions about the Progress Notes form can lead to confusion and errors in documentation. Here are five common misunderstandings:
- It is only for doctors to fill out. Many believe that only physicians are responsible for completing Progress Notes. In reality, all healthcare providers involved in a patient's care can and should contribute to these notes.
- Progress Notes are optional. Some think that filling out Progress Notes is not mandatory. However, these notes are crucial for maintaining accurate medical records and ensuring continuity of care.
- They are only for serious cases. There is a misconception that Progress Notes are only necessary for critical or complicated cases. In truth, they are important for every patient encounter, regardless of the severity of the condition.
- Progress Notes do not need to be detailed. A common belief is that brief notes are sufficient. However, detailed documentation is essential for clarity and to provide a comprehensive view of the patient's progress and treatment.
- Once completed, they cannot be modified. Some individuals think that Progress Notes are final and cannot be changed. In fact, they can be amended if new information arises or corrections are needed, but this must be done following proper protocols.
Documents used along the form
In healthcare settings, various forms and documents work together to ensure comprehensive patient care. Each document serves a specific purpose, contributing to a clear understanding of a patient’s medical history and treatment plan. Below is a list of commonly used forms alongside the Progress Notes form.
- Patient Intake Form: This document collects essential information about a patient’s medical history, current medications, and personal details. It helps healthcare providers understand the patient’s background before the first appointment.
- Consent Form: Patients sign this form to give permission for specific medical treatments or procedures. It ensures that patients are informed about the risks and benefits involved in their care.
- Treatment Plan: This outline details the proposed course of treatment for a patient. It includes goals, interventions, and timelines, guiding healthcare providers in delivering consistent care.
- Discharge Summary: Created when a patient leaves a healthcare facility, this summary provides a recap of the patient's treatment, progress, and any follow-up care needed. It ensures continuity of care after discharge.
- Referral Form: This document is used when a healthcare provider refers a patient to a specialist. It includes relevant patient information and the reason for the referral, facilitating effective communication between providers.
- Medication Administration Record (MAR): This record tracks all medications administered to a patient during their stay. It helps prevent errors and ensures that patients receive their medications as prescribed.
- Lab Results Report: This document contains the findings from laboratory tests performed on a patient. It is crucial for diagnosing conditions and determining appropriate treatment plans.
- Power of Attorney Form: To ensure your decisions are honored, complete the Texas Power of Attorney document for your legal needs.
- Follow-Up Appointment Form: This form schedules future appointments and outlines any necessary preparations for the patient. It ensures that patients continue to receive care after their initial visit.
These documents, along with the Progress Notes form, create a comprehensive system for managing patient care. Each one plays a vital role in ensuring that healthcare providers have the necessary information to make informed decisions about treatment and support patient well-being.
Steps to Filling Out Progress Notes
Filling out the Progress Notes form is an important step in documenting patient care. By following these steps, you will ensure that all necessary information is accurately recorded for future reference.
- Date: Write the date of the entry at the top of the form. Make sure to use the correct format, typically MM/DD/YYYY.
- Patient's Identification: Fill in the patient's name, including last, first, and middle name. Include their grade, rank, rate, and the name of the hospital or medical facility where they are receiving care.
- Register Number: Enter the patient’s register number in the designated space. This number is crucial for tracking the patient's medical records.
- Ward Number: Indicate the ward number where the patient is being treated. This helps in locating the patient within the facility.
- Progress Notes: Write detailed notes about the patient's condition, treatment, and any observations. Be clear and concise to ensure the information is easily understood.
After completing the form, review all entries for accuracy. Ensure that everything is filled out completely before submitting it as part of the patient's medical record.
Common mistakes
-
Failing to include the date on the Progress Notes form can lead to confusion about when the notes were made. It is essential to document the date accurately.
-
Omitting the patient's identification details, such as name, grade, and hospital or medical facility, can make it difficult to associate the notes with the correct patient.
-
Not using the correct register number and ward number can result in misfiling or miscommunication among healthcare providers.
-
Writing vague or unclear progress notes can hinder the understanding of the patient's condition and treatment. Specificity is crucial.
-
Neglecting to continue notes on the reverse side when more space is needed can lead to incomplete documentation.
-
Using abbreviations or jargon that are not universally understood can create misunderstandings. Clear language should always be prioritized.
-
Forgetting to sign or initial the notes can raise questions about accountability and authenticity.
-
Failing to update the notes regularly can result in outdated information being used for patient care decisions. Regular updates are vital for effective treatment.
Get Clarifications on Progress Notes
What is the purpose of the Progress Notes form?
The Progress Notes form serves as a vital tool in medical record-keeping. It documents a patient's ongoing treatment and progress over time. This information is essential for healthcare providers to track the effectiveness of interventions and make informed decisions about future care.
Who should fill out the Progress Notes form?
Healthcare professionals involved in a patient's care are responsible for completing the Progress Notes form. This includes doctors, nurses, and therapists. Each entry should reflect their observations, assessments, and any changes in the patient's condition.
What information is required on the Progress Notes form?
Key details must be included to ensure the form is complete. This includes:
- Patient's full name (last, first, middle)
- Grade, rank, or rate of the patient
- Hospital or medical facility name
- Patient's identification number and ward number
- Date of the entry
How often should Progress Notes be completed?
Progress Notes should be filled out regularly, typically during each patient visit or whenever there is a significant change in the patient's condition. Consistency is key to maintaining an accurate and up-to-date medical record.
Can Progress Notes be completed electronically?
Yes, many healthcare facilities now allow for electronic completion of Progress Notes. This can enhance efficiency and improve the accessibility of patient records. However, it is essential to ensure that electronic systems comply with relevant privacy and security regulations.
What should be done if an error is made on the Progress Notes form?
If an error occurs, it is important to correct it properly. Cross out the mistake with a single line, and initial the correction. Avoid using white-out or erasing the error, as this could lead to confusion and questions about the accuracy of the record.
Are there specific guidelines for writing Progress Notes?
While guidelines can vary by institution, some general best practices include:
- Be clear and concise in your writing.
- Use objective language and avoid subjective opinions.
- Document any assessments, interventions, and patient responses.
- Ensure that entries are dated and signed by the person making them.
What is the importance of maintaining confidentiality in Progress Notes?
Confidentiality is crucial when handling Progress Notes. These documents contain sensitive patient information that must be protected to comply with privacy laws. Ensuring that only authorized personnel have access to these records helps maintain trust between patients and healthcare providers.