Fill in a Valid Prescription Pad Form
Common PDF Forms
Texas Temporary Tag - The temporary tag is a practical solution for individuals dealing with unexpected delays in registration.
Form 6059B Customs Declaration - The CBP 6059B also provides guidelines about the items prohibited or restricted in the U.S.
The FedEx Release Authorization form is a crucial document for individuals expecting a delivery but unable to be present at the delivery location. It allows the recipient to indicate a preferred location where FedEx can leave the package, ensuring the delivery process is not hindered by their absence. However, it's important to note that a valid signature is necessary for the delivery, and a separate form is needed for each package, highlighting the form's role in maintaining the delivery's security and accountability. For further information, you can visit https://toptemplates.info.
Western Union Receipt - Benefit from a long history of reliable service.
Misconceptions
Understanding the Prescription Pad form is essential for both healthcare providers and patients. However, several misconceptions can lead to confusion. Below is a list of common misconceptions and clarifications regarding the Prescription Pad form.
- The Prescription Pad form is only for medications. Many people believe that the form is exclusively for prescribing medications. In reality, it can also include instructions for therapies, medical devices, or other treatments.
- Only doctors can use the Prescription Pad form. While physicians are the primary users, other licensed healthcare providers, such as nurse practitioners and physician assistants, can also issue prescriptions using this form.
- All prescriptions must be handwritten. Some think that prescriptions can only be written by hand. In fact, electronic prescriptions are widely accepted and often preferred for their accuracy and efficiency.
- Once a prescription is written, it cannot be changed. Many assume that prescriptions are final once written. However, healthcare providers can modify or cancel prescriptions as needed, following proper protocols.
- Patients cannot ask questions about their prescriptions. It is a common belief that patients should not question their prescriptions. In truth, patients are encouraged to ask questions to ensure they understand their treatment.
- The Prescription Pad form is the same in every state. Some individuals think that all states use a uniform Prescription Pad form. Each state has its own regulations and requirements, which can affect the form's design and usage.
- Prescriptions are only valid for a short time. There is a misconception that all prescriptions expire quickly. While some prescriptions have specific expiration dates, others, especially for chronic conditions, may be valid for longer periods.
- Only certain medications can be prescribed using this form. Some believe that the form is limited to specific medications. In reality, it can be used for a wide range of treatments, depending on the healthcare provider's judgment.
- Once a prescription is filled, it cannot be refilled. Many think that refills are not an option after a prescription is filled. However, refills can be authorized by the prescribing healthcare provider if appropriate.
By addressing these misconceptions, individuals can better navigate the Prescription Pad form and understand its purpose in the healthcare process.
Documents used along the form
In the medical field, various forms and documents complement the Prescription Pad form, each serving a unique purpose in patient care and medication management. Understanding these documents is essential for healthcare professionals to ensure compliance with regulations and to promote patient safety.
- Patient Intake Form: This document collects essential information about a patient, including their medical history, current medications, allergies, and contact information. It serves as the foundation for the healthcare provider's understanding of the patient's health status.
- Medication Administration Record (MAR): The MAR is used to track the administration of medications to patients. It includes details such as the medication name, dosage, route, and time of administration, ensuring that patients receive their medications as prescribed.
- Informed Consent Form: This form is crucial for obtaining a patient's consent before administering certain treatments or medications. It outlines the risks, benefits, and alternatives, allowing patients to make informed decisions about their healthcare.
- Refill Authorization Request: When a patient needs a refill on their prescription, this document is used to request authorization from the prescribing provider. It helps maintain continuity of care and ensures that patients do not run out of necessary medications.
- IRS 2553 Form: The https://smarttemplates.net/fillable-irs-2553 is essential for small businesses to elect S corporation status, facilitating potential tax savings through pass-through taxation.
- Drug Utilization Review (DUR): This document is a systematic process to evaluate prescribed medications for appropriateness, safety, and effectiveness. It helps identify potential drug interactions and ensures that the prescribed medications align with clinical guidelines.
- Prescription Drug Monitoring Program (PDMP) Report: Many states maintain a PDMP to track prescriptions of controlled substances. This report helps providers monitor patient prescriptions, reducing the risk of misuse and ensuring responsible prescribing practices.
- Clinical Notes: These notes are written by healthcare providers during patient visits. They document the patient's condition, treatment plans, and any changes in medication, serving as a vital communication tool among healthcare team members.
- Discharge Summary: Upon a patient's discharge from a healthcare facility, this summary outlines the patient's treatment, medications prescribed, and follow-up care instructions. It ensures that patients and their caregivers understand the next steps in their care.
- Prior Authorization Form: Some insurance companies require this form before they will cover certain medications. It documents the medical necessity of the prescribed drug and helps streamline the insurance approval process.
Each of these documents plays a significant role in the healthcare system, working together to enhance patient safety, ensure effective communication, and promote adherence to treatment plans. Familiarity with these forms can help healthcare professionals provide better care and navigate the complexities of patient management.
Steps to Filling Out Prescription Pad
Filling out the Prescription Pad form requires careful attention to detail. The following steps will guide you through the process, ensuring that all necessary information is accurately recorded.
- Start by entering the patient's full name at the top of the form.
- Next, fill in the patient's date of birth to confirm their identity.
- Provide the patient's address, including street, city, state, and ZIP code.
- Indicate the date on which the prescription is being issued.
- Write the name of the medication being prescribed, including the dosage and form (e.g., tablet, liquid).
- Specify the quantity of the medication to be dispensed.
- Include any special instructions for the patient regarding the medication.
- Sign the form with your name and credentials as the prescribing provider.
- Finally, ensure that the form is legible and free from any errors before submitting it.
Common mistakes
-
Incomplete Patient Information: Failing to provide all necessary details about the patient can lead to delays in processing. Always include the patient's full name, date of birth, and contact information.
-
Incorrect Medication Details: Double-check the medication name, dosage, and frequency. Typos or incorrect information can result in serious health risks.
-
Missing Signature: A prescription must be signed by the prescribing physician. Without a signature, the prescription may not be valid.
-
Not Including Refills: If refills are needed, specify the number allowed. Omitting this detail can lead to confusion for both the pharmacy and the patient.
-
Failure to Indicate Special Instructions: If there are specific instructions for the medication, such as how to take it or potential side effects, include them. This information is crucial for patient safety.
-
Using Abbreviations: While some abbreviations are standard, using too many can create misunderstandings. Clear communication is essential.
-
Neglecting to Update Information: If a patient's information changes, such as their address or insurance, ensure that the prescription reflects these updates.
-
Not Reviewing Before Submission: Always take a moment to review the completed form. A quick check can prevent many common mistakes.
Get Clarifications on Prescription Pad
What is a Prescription Pad form?
A Prescription Pad form is a document used by healthcare providers to prescribe medication to patients. It typically includes the patient's information, the prescribed medication, dosage, and instructions for use. This form is essential for ensuring that patients receive the correct treatment as intended by their healthcare provider.
Who can issue a Prescription Pad form?
Only licensed healthcare professionals, such as doctors, nurse practitioners, and physician assistants, can issue a Prescription Pad form. These professionals have the authority to evaluate patients and determine appropriate medications based on their medical needs.
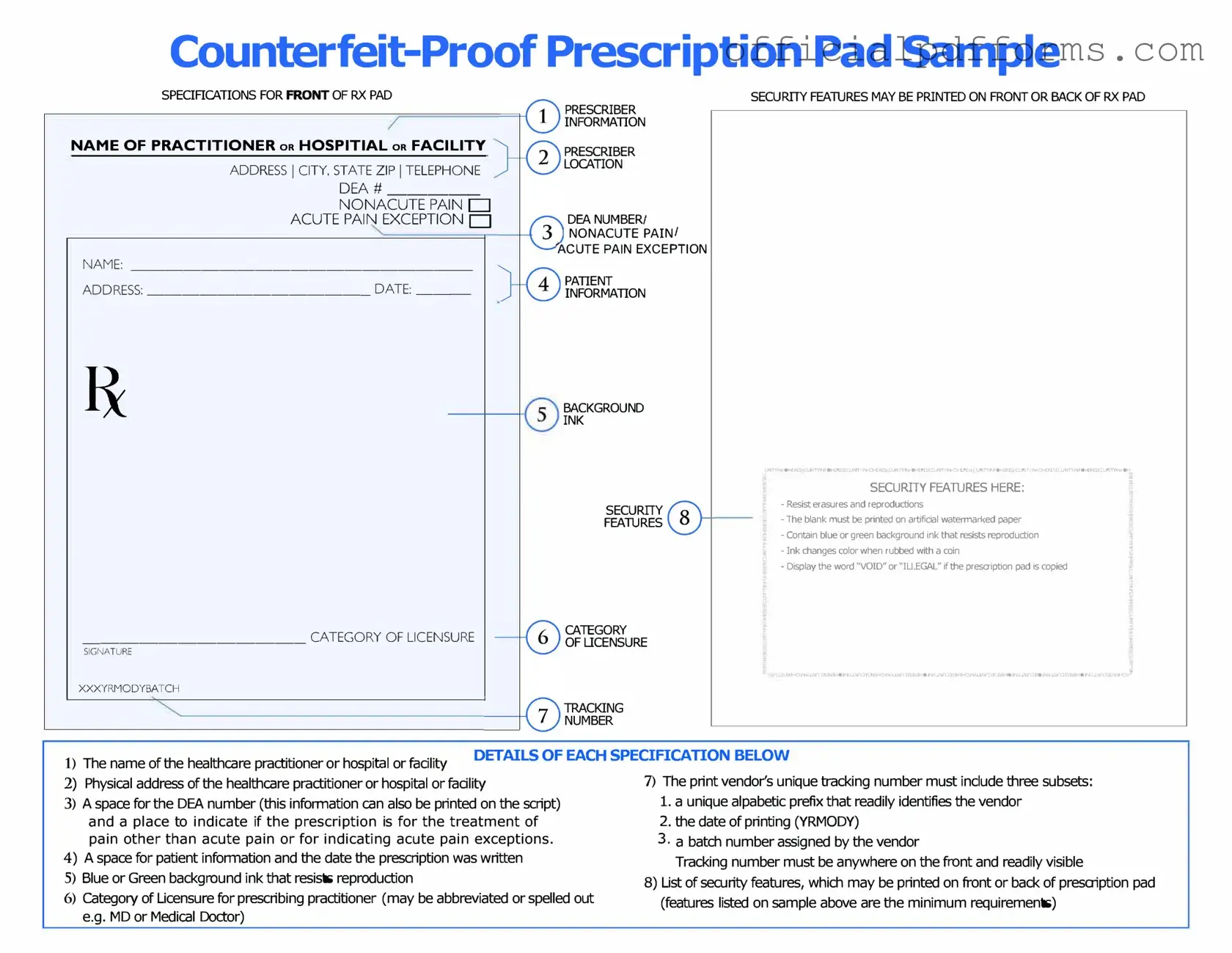
What information is required on a Prescription Pad form?
A typical Prescription Pad form should include the following information:
- Patient's name and contact information
- Provider's name, contact information, and signature
- Date of the prescription
- Medication name, dosage, and form (e.g., tablet, liquid)
- Instructions for use (e.g., frequency, duration)
- Refill information, if applicable
Including all these details helps prevent errors and ensures that the pharmacy can fill the prescription correctly.
Can a Prescription Pad form be used for controlled substances?
Yes, a Prescription Pad form can be used for controlled substances, but there are specific regulations that must be followed. Providers must comply with federal and state laws regarding the prescribing of controlled substances. This may include using special prescription pads that are tamper-resistant and include unique identifiers.
How long is a Prescription Pad form valid?
The validity of a Prescription Pad form varies by state and the type of medication prescribed. Generally, a prescription for non-controlled substances may be valid for up to one year, while prescriptions for controlled substances often have shorter validity periods, typically ranging from 5 to 30 days. Always check local regulations for specific guidelines.
What should I do if I lose my Prescription Pad form?
If a Prescription Pad form is lost, it is crucial to notify your healthcare provider immediately. They may need to issue a new prescription to prevent unauthorized use. Additionally, if the prescription was for a controlled substance, reporting the loss to local authorities may be necessary to prevent potential misuse.