Fill in a Valid Medication Administration Record Sheet Form
Common PDF Forms
Military Awards After Discharge - The DD 149 is a pivotal document for military members aiming for justice in their records.
Lyft Inspection Form Sc - Verify that all lights, including headlights and brake lights, are functioning properly.
For those looking to understand more about the importance of an Operating Agreement in business operations, this resource provides a comprehensive overview. It details how this document can facilitate smoother management and reduce conflicts among members. To access a free template, simply visit your essential Operating Agreement guide.
Gift Certificate Templates - Perfect for coworkers, this gift certificate shows appreciation without the fuss.
Misconceptions
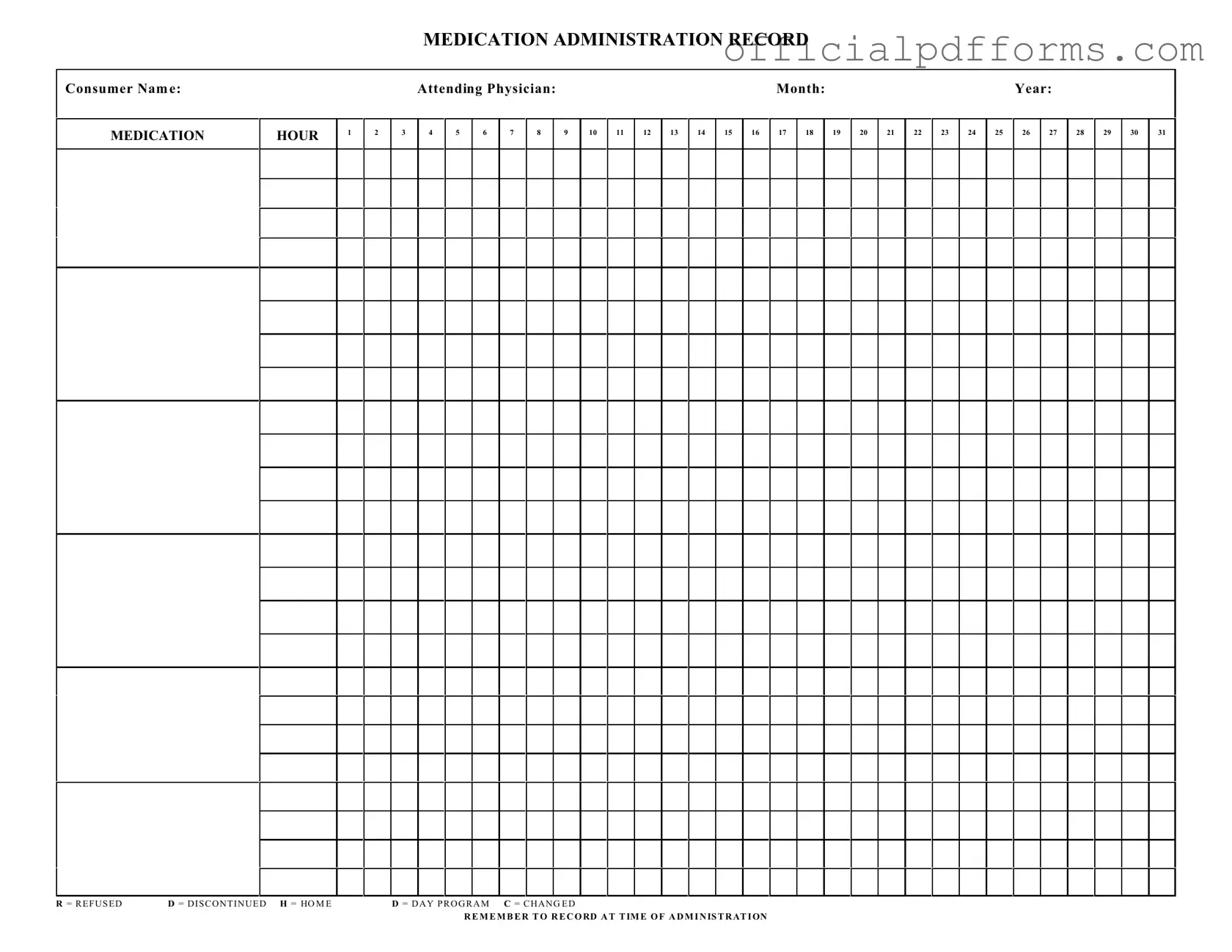
Understanding the Medication Administration Record Sheet (MARS) is crucial for ensuring proper medication management. However, several misconceptions can lead to confusion. Here are five common misconceptions:
- 1. The MARS is only for nurses. Many believe that only nursing staff should handle the MARS. In reality, anyone involved in medication administration, including caregivers and support staff, should understand how to use this form effectively.
- 2. The MARS is optional. Some individuals think that using the MARS is not mandatory. This is not true. Accurate documentation is essential for patient safety and is often required by healthcare regulations.
- 3. You can fill out the MARS at any time. It's a common belief that the MARS can be completed at any point during the day. However, it must be filled out at the time of administration to ensure accuracy and accountability.
- 4. Abbreviations on the MARS are universally understood. While certain abbreviations may seem standard, not everyone interprets them the same way. It's vital to clarify any abbreviations used to avoid misunderstandings.
- 5. The MARS is just a checklist. Some view the MARS as merely a checklist for medications. In fact, it serves as a critical communication tool that helps track patient medication history and informs all healthcare providers involved in the patient's care.
Clearing up these misconceptions can enhance the effectiveness of medication administration and improve patient outcomes. Understanding the proper use of the MARS is essential for everyone involved in the healthcare process.
Documents used along the form
The Medication Administration Record Sheet is a crucial document used in healthcare settings to track the administration of medications to patients. Along with this form, several other documents are commonly utilized to ensure proper medication management and patient care. Below is a list of four additional forms and documents that often accompany the Medication Administration Record Sheet.
- Medication Order Form: This document provides the specific instructions from a physician regarding the medications a patient should receive. It includes details such as the medication name, dosage, frequency, and any special instructions. This form is essential for ensuring that healthcare providers administer the correct medication as prescribed.
- Recommendation Letter Form: This structured template is essential for endorsing an individual's capabilities and character in various settings. Often required for academic admissions and job applications, it enables referees to effectively communicate their insights into the applicant's qualifications, providing a comprehensive picture of their potential. For more details, visit OnlineLawDocs.com.
- Patient Consent Form: Before administering certain medications, especially those with potential side effects, healthcare providers often require a patient or guardian's consent. This form outlines the medication, its purpose, potential risks, and benefits. It ensures that the patient is informed and agrees to the treatment plan.
- Medication Reconciliation Form: This document is used to compare a patient's current medication list with the medications they are prescribed during their healthcare visits. It helps identify any discrepancies, such as omissions or duplications, ensuring that patients receive the correct medications throughout their treatment.
- Incident Report Form: If there is an adverse reaction or error related to medication administration, an incident report must be completed. This form documents the details of the incident, including what happened, who was involved, and any actions taken in response. It serves as a critical tool for improving safety and preventing future occurrences.
These documents work together with the Medication Administration Record Sheet to promote safe and effective medication management. Proper use of these forms helps healthcare providers maintain accurate records and ensures that patients receive the best possible care.
Steps to Filling Out Medication Administration Record Sheet
Filling out the Medication Administration Record Sheet is an important task that ensures accurate tracking of medication administration for each consumer. This process requires careful attention to detail to avoid errors and ensure compliance with medical protocols. Follow the steps outlined below to complete the form effectively.
- Begin by entering the Consumer Name at the top of the form.
- Next, write the Attending Physician's Name in the designated space.
- Fill in the Month and Year in the appropriate sections.
- Identify the Medication Hour by marking the corresponding hour for each medication administration.
- Record the medication administration for each day of the month by filling in the appropriate boxes with either a checkmark or initials.
- If a dose is refused, indicate this by writing R in the corresponding box.
- If a medication is discontinued, write D in the relevant box.
- For medications that are taken at home, mark H.
- For medications administered during a day program, use D.
- If there is a change in the medication, record C in the appropriate space.
- Finally, remember to record the time of administration next to each entry to maintain accurate records.
Common mistakes
-
Not including the consumer name. Always ensure the consumer's name is clearly stated at the top of the form. This helps in identifying the correct individual for medication administration.
-
Failing to document the attending physician. It’s essential to include the name of the physician responsible for the consumer’s care. This provides clarity and accountability.
-
Omitting the date. Always fill in the month and year. This is crucial for tracking medication over time and ensuring proper record-keeping.
-
Not recording the time of administration. Each medication should be documented at the time it is given. This helps in maintaining accurate records and monitoring the consumer's response.
-
Using unclear abbreviations. Make sure to use standard abbreviations like R for Refused, D for Discontinued, and H for Home. Avoid confusion by ensuring everyone understands the terms used.
-
Neglecting to indicate changes in medication. If a medication has changed, it should be clearly noted on the record. This is vital for ongoing treatment and care.
Get Clarifications on Medication Administration Record Sheet
What is the purpose of the Medication Administration Record Sheet?
The Medication Administration Record Sheet is designed to track the administration of medications to consumers. It ensures that all medications are given at the correct times and allows healthcare providers to monitor any refusals or changes in medication regimens.
Who is responsible for filling out the Medication Administration Record Sheet?
Typically, the healthcare provider or nurse administering the medication is responsible for completing the form. They must accurately record the time of administration, any refusals, and any changes to the medication as directed by the attending physician.
How should I record a refused medication?
If a consumer refuses to take their medication, the provider should mark an "R" on the corresponding date and time on the record sheet. It is important to document the refusal clearly and to follow up as necessary to ensure the consumer's health and safety.
What does it mean if a medication is marked as discontinued?
A medication marked with a "D" indicates that it has been discontinued. This could be due to a variety of reasons, such as a change in the treatment plan or side effects. It is crucial to ensure that all healthcare team members are aware of any discontinued medications to prevent errors.
How do I indicate a change in medication?
To indicate a change in medication, write a "C" next to the date and time of administration on the record sheet. Additionally, it is advisable to provide a brief note or explanation regarding the change to maintain clear communication among the healthcare team.
What should I do if I forget to record a medication administration?
If you forget to record a medication administration, make sure to note it as soon as you realize the oversight. Document the time and date it should have been recorded, and provide an explanation if necessary. Consistency in record-keeping is vital for patient safety.
How often should the Medication Administration Record Sheet be updated?
The Medication Administration Record Sheet should be updated each time medication is administered. This includes recording refusals, changes, and any other relevant information. Regular updates help ensure that the consumer's medication history is accurate and current.
Can the Medication Administration Record Sheet be used for multiple consumers?
No, each consumer should have their own Medication Administration Record Sheet. This practice helps maintain confidentiality and ensures that each individual's medication history is accurately tracked without confusion.
What information is required on the Medication Administration Record Sheet?
The form requires the following information:
- Consumer's name
- Attending physician's name
- Month and year of administration
- Time of medication administration
- Any refusals, changes, or discontinuations marked appropriately
Where should I keep the completed Medication Administration Record Sheets?
Completed Medication Administration Record Sheets should be stored securely in a designated location, such as a medical record file or electronic health record system. Ensure that access is limited to authorized personnel to maintain patient confidentiality.