Valid Do Not Resuscitate Order Document
Do Not Resuscitate Order Forms for Individual US States
Fill out Popular Documents
Eagle Scout Recommendation Letter Sample - Through stories and reflections, this recommendation brings to life the candidate's journey toward becoming an Eagle Scout.
Cadet Command - Cadets must reflect on their progress to achieve academic and ROTC objectives.
For individuals looking to understand their options, an overview of the key Texas RV Bill of Sale requirements is invaluable. This document not only serves to facilitate the sale process but also ensures that both buyers and sellers fulfill their responsibilities effectively. To learn more about this essential document, visit our guide on the important RV Bill of Sale.
Home Load Calculation - It establishes a benchmark for evaluating existing electrical load against code requirements.
Misconceptions
Understanding the Do Not Resuscitate (DNR) Order can be challenging. Here are seven common misconceptions about DNR forms:
-
A DNR means no medical care will be provided.
This is false. A DNR only indicates that resuscitation efforts should not be made in the event of cardiac arrest. Other medical treatments and care continue as needed.
-
Only terminally ill patients can have a DNR.
This is not true. While many people with terminal illnesses choose DNR orders, anyone can request one based on their personal health care preferences.
-
A DNR is the same as a living will.
This is a misconception. A living will outlines a person's wishes regarding medical treatments in general, while a DNR specifically addresses resuscitation efforts.
-
DNR orders are only for hospitals.
This is incorrect. DNR orders can be established for use in various settings, including homes and long-term care facilities.
-
A DNR can be ignored by medical personnel.
This is false. Medical professionals are legally obligated to honor a valid DNR order. Ignoring it can lead to legal consequences.
-
You cannot change your mind once a DNR is in place.
This is not accurate. Individuals can revoke or modify a DNR order at any time, as long as they are competent to do so.
-
A DNR means you will die immediately.
This is misleading. A DNR does not hasten death; it simply allows natural processes to occur without interference from resuscitation efforts.
Documents used along the form
A Do Not Resuscitate (DNR) Order is a crucial document for individuals who wish to express their preferences regarding resuscitation efforts in the event of a medical emergency. However, several other forms and documents are often used alongside a DNR to ensure that a person's healthcare wishes are clearly communicated and respected. Below is a list of these important documents.
- Advance Healthcare Directive: This document allows individuals to outline their preferences for medical treatment in advance. It can include instructions about life-sustaining treatments, including resuscitation, and appoints a healthcare proxy to make decisions on their behalf if they are unable to do so.
- Healthcare Power of Attorney: This legal document designates someone to make medical decisions for an individual if they become incapacitated. It provides clarity on who can act on behalf of the patient in critical situations.
- Living Will: A living will details specific medical treatments an individual does or does not want in the event of a terminal illness or irreversible condition. It complements a DNR by specifying preferences for end-of-life care.
- Texas Motor Vehicle Bill of Sale: This document serves as a record of sale and transfer of ownership of a motor vehicle, protecting both parties involved. For more information, visit OnlineLawDocs.com.
- Physician Orders for Life-Sustaining Treatment (POLST): This form translates a patient’s wishes regarding treatment into actionable medical orders. It is especially useful for individuals with serious health conditions and ensures their preferences are followed by healthcare providers.
- Do Not Intubate (DNI) Order: Similar to a DNR, a DNI order specifically states that a patient does not wish to be intubated or placed on a ventilator. This document can be part of a broader advance directive or a standalone form.
- Medical History and Medication List: This document provides healthcare providers with a comprehensive overview of a patient’s medical history and current medications. It is essential for making informed decisions about treatment options and respecting the patient's wishes.
Having these documents in place helps ensure that healthcare providers understand and respect an individual's wishes regarding medical treatment. They provide clarity and guidance in critical moments, allowing individuals to maintain control over their healthcare decisions.
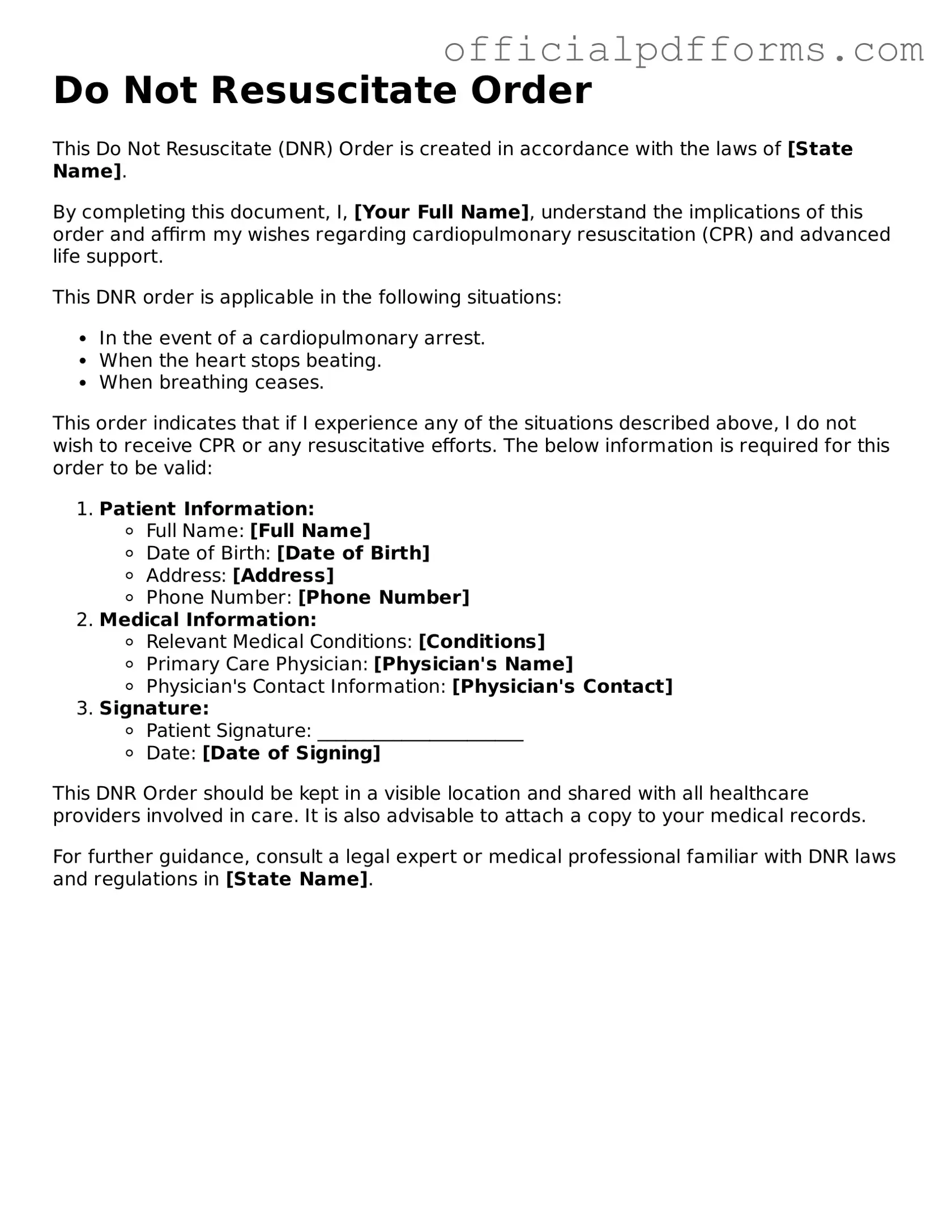
Steps to Filling Out Do Not Resuscitate Order
Filling out a Do Not Resuscitate (DNR) Order form is an important step for individuals who wish to outline their preferences regarding medical treatment in emergency situations. This process involves careful consideration and clear communication of your wishes. Below are the steps to complete the form accurately.
- Obtain the DNR Order form from a healthcare provider or download it from a trusted medical website.
- Read the instructions carefully to understand the requirements and implications of the form.
- Begin by filling out your personal information, including your full name, date of birth, and contact information.
- Identify your healthcare provider by entering their name and contact details. This helps ensure your wishes are communicated effectively.
- Clearly state your wishes regarding resuscitation. This may involve checking a box or writing a statement, depending on the form's design.
- Include any additional instructions or preferences you may have regarding your medical care.
- Sign and date the form to validate your choices. This step is crucial as it confirms that the decisions reflect your intentions.
- Have a witness sign the form if required. Some states mandate a witness to ensure the legitimacy of your request.
- Make copies of the completed form for your records and share it with your healthcare provider and family members.
After completing the form, it’s essential to keep it in a location that is easily accessible. Discuss your wishes with your loved ones and healthcare team to ensure everyone understands your preferences. This proactive approach can provide peace of mind and clarity in critical situations.
Common mistakes
-
Not discussing the decision with family members. One common mistake is failing to have an open conversation with loved ones about the decision to fill out a Do Not Resuscitate (DNR) Order. This can lead to confusion and emotional distress during a critical time.
-
Not understanding the implications of a DNR. Some individuals may fill out the form without fully grasping what it means. It is essential to know that a DNR order specifically instructs medical personnel not to perform cardiopulmonary resuscitation (CPR) in case of cardiac arrest.
-
Inaccurate or incomplete information. Filling out the form incorrectly can lead to complications. Ensure that all personal information, such as name, date of birth, and medical conditions, is accurately provided to avoid any misunderstandings.
-
Failing to update the form. Life circumstances change, and so do health conditions. It is crucial to revisit and update the DNR order regularly, especially after significant health changes or hospitalizations.
-
Not discussing the DNR with healthcare providers. After completing the DNR form, individuals often forget to share it with their healthcare team. This can lead to situations where medical staff may not be aware of the patient's wishes, potentially resulting in unwanted interventions.
Get Clarifications on Do Not Resuscitate Order
What is a Do Not Resuscitate Order (DNR)?
A Do Not Resuscitate Order is a legal document that allows a person to refuse resuscitation efforts in case of cardiac arrest or respiratory failure. This order is typically used by individuals with serious health conditions who wish to avoid aggressive medical interventions that may not align with their goals of care.
Who can request a DNR?
Generally, any adult who is capable of making their own medical decisions can request a DNR. This includes patients with terminal illnesses or those who are in advanced stages of chronic diseases. Family members or legal guardians may also request a DNR on behalf of someone who is unable to make decisions for themselves.
How is a DNR order created?
To create a DNR order, a conversation with a healthcare provider is necessary. The provider will assess the individual's health condition and discuss the implications of a DNR. Once both parties agree, the provider will complete the DNR form, which must be signed by the patient and the physician. In some states, a witness may also be required.
Is a DNR order legally binding?
Yes, a properly executed DNR order is legally binding. Healthcare providers are required to follow the order in emergency situations. However, it’s essential to ensure that the DNR is recognized in the state where the patient is receiving care, as laws and regulations may vary by state.
Can a DNR order be revoked?
Yes, a DNR order can be revoked at any time. The individual who signed the order can verbally communicate their wish to revoke it, or they can create a new document that explicitly states the revocation. It is advisable to inform healthcare providers and family members of the change to ensure that the new wishes are respected.
What happens if a DNR order is not honored?
If a DNR order is not honored, it can lead to legal complications for the healthcare providers involved. Patients or their families may have grounds for a complaint or lawsuit if they believe their wishes were ignored. It is crucial for individuals to ensure that their DNR orders are clearly communicated and readily available to medical personnel.
Where should I keep my DNR order?
It is important to keep the DNR order in a place that is easily accessible. Common recommendations include:
- Keeping a copy in the patient’s medical file.
- Providing copies to family members and caregivers.
- Displaying a copy prominently in the home, such as on the refrigerator or near the front door.
Having multiple copies ensures that healthcare providers can quickly access the order when needed.