Fill in a Valid Cna Shower Sheets Form
Common PDF Forms
Facial Consent Form Template - Understand how to manage any post-treatment concerns.
When entering into a rental agreement, it is important for both landlords and tenants to be well-informed about the California Lease Agreement form, which serves as a foundation for the rental relationship. To ensure compliance with legal standards and avoid conflicts, it is advisable for renters and property owners to thoroughly review the document and its stipulations. For those looking to secure a legally sound agreement, you can find the form here to streamline the process and clarify essential terms.
Marriage Records Sacramento Ca - Obtaining a certified copy may be necessary for certain purposes.
Misconceptions
Misconceptions about the CNA Shower Sheets form can lead to misunderstandings in its use and purpose. Below are ten common misconceptions along with clarifications.
- The form is only for reporting serious skin issues. Many believe that the form is only necessary for severe conditions. In reality, it is essential for documenting all skin abnormalities, regardless of severity.
- Only licensed nurses can complete the form. While charge nurses review the form, certified nursing assistants (CNAs) are trained to fill it out based on their assessments.
- The body chart is optional. Some think that the body chart is not necessary. However, it is crucial for accurately locating and describing skin issues.
- The form is only for use during showers. This misconception overlooks that the form can be used anytime a visual skin assessment is performed, not just during bathing.
- Abnormalities must be reported only if they are new. It is important to report any changes in a resident's skin condition, whether new or existing.
- Documentation is not necessary if there are no visible issues. Even if no abnormalities are found, completing the form is still necessary for maintaining accurate records.
- All skin conditions require immediate intervention. Not every abnormality necessitates immediate action; some may require monitoring and follow-up.
- The form is only for the CNA's use. The information on the form is vital for the entire care team, including charge nurses and the Director of Nursing (DON).
- Skin assessments are not important. This misconception undermines the importance of regular skin assessments in preventing complications.
- The form is outdated and not relevant. Despite its age, the form is still a useful tool for documenting skin assessments and ensuring resident care quality.
Documents used along the form
The CNA Shower Sheets form is essential for documenting skin assessments during resident showers. Several other forms and documents complement this process, ensuring comprehensive care and communication among staff. Below is a list of these important documents.
- Incident Report: This document records any unexpected events or accidents that occur during care. It includes details about what happened, the individuals involved, and any immediate actions taken.
- Care Plan: A personalized plan that outlines the specific needs and preferences of each resident. It details the interventions required to meet their health and wellness goals.
- Daily Progress Notes: These notes provide a summary of a resident's condition and any changes observed throughout the day. They are crucial for tracking health trends over time.
- Recommendation Letter Form: This form can provide valuable insights into a candidate's abilities and character, strengthening their application in competitive environments. For templates and guidance, visit toptemplates.info/.
- Medication Administration Record (MAR): This form tracks all medications administered to a resident, including dosages and times. It ensures accurate medication management and compliance.
- Skin Assessment Form: Used for a more detailed evaluation of skin conditions, this form documents specific findings and any necessary follow-up actions.
- Vital Signs Record: This document logs the resident's vital signs, such as temperature, pulse, and blood pressure. Regular monitoring helps identify potential health issues early.
- Transfer Form: When a resident is moved to another facility or unit, this form provides essential information about their care needs and medical history to ensure continuity of care.
- Family Communication Log: This log documents all interactions with a resident's family members, including updates on the resident's condition and any concerns raised by the family.
Utilizing these forms effectively enhances the quality of care provided to residents. Each document plays a crucial role in maintaining clear communication and ensuring that all staff members are informed about the residents' needs and conditions.
Steps to Filling Out Cna Shower Sheets
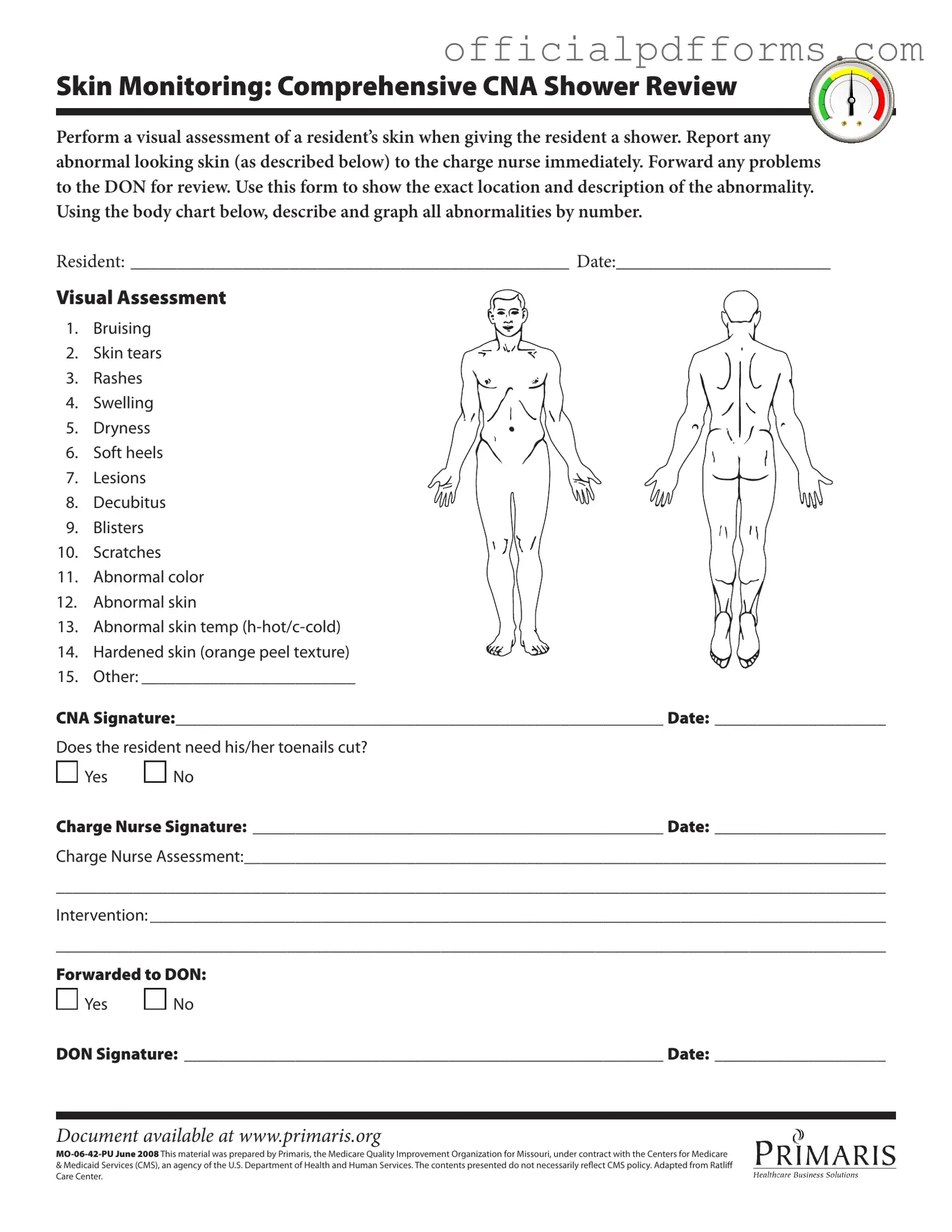
Completing the CNA Shower Sheets form is essential for documenting skin assessments during resident showers. This process ensures that any abnormalities are reported and addressed promptly. Follow the steps below to accurately fill out the form.
- Begin by entering the resident's name in the space labeled RESIDENT.
- Fill in the date of the assessment in the DATE section.
- Conduct a visual assessment of the resident's skin while giving the shower.
- Identify any abnormalities from the list provided, such as bruising, rashes, or lesions.
- Use the body chart to mark the exact location of each abnormality by number.
- In the space labeled Other, describe any additional abnormalities that are not listed.
- Sign the form in the CNA Signature section and include the date.
- Determine if the resident needs toenail trimming. Circle Yes or No accordingly.
- Have the charge nurse sign the form in the Charge Nurse Signature section and include the date.
- In the Charge Nurse Assessment area, provide detailed notes about the assessment findings.
- Document any interventions required in the Intervention section.
- Indicate if the report has been forwarded to the Director of Nursing (DON) by circling Yes or No.
- If forwarded, have the DON sign the form and include the date.
Common mistakes
-
Inadequate Visual Assessment: A common mistake is failing to conduct a thorough visual assessment of the resident's skin. Each area of the skin should be carefully examined for any abnormalities. Skipping this step can lead to undetected issues that may worsen over time.
-
Neglecting to Report Abnormalities: It is crucial to report any findings of abnormal skin to the charge nurse immediately. Some individuals may hesitate or forget to communicate these issues, which can delay necessary interventions and potentially harm the resident's health.
-
Incorrect Documentation: Accurately documenting the location and description of any abnormalities is essential. Mislabeling or failing to use the body chart correctly can lead to confusion and miscommunication among the care team.
-
Ignoring Additional Notes: The form allows for additional notes regarding the resident's condition. Failing to utilize this section can result in overlooking important details that might inform further care or interventions.
-
Not Following Up: After completing the form, it is vital to ensure that any issues are forwarded to the Director of Nursing (DON) as required. Neglecting this step can impede the overall care process and may leave the resident at risk.
Get Clarifications on Cna Shower Sheets
What is the purpose of the CNA Shower Sheets form?
The CNA Shower Sheets form is designed to assist certified nursing assistants (CNAs) in performing a thorough visual assessment of a resident's skin during showering. It serves as a documentation tool to report any abnormalities, ensuring that issues are communicated to the charge nurse and, if necessary, the Director of Nursing (DON). By using this form, CNAs can accurately record the location and description of any skin problems, which is crucial for the resident's ongoing care.
What types of skin abnormalities should be monitored?
During the shower assessment, CNAs should be vigilant for various skin abnormalities, including:
- Bruising
- Skin tears
- Rashes
- Swelling
- Dryness
- Soft heels
- Lesions
- Decubitus (pressure ulcers)
- Blisters
- Scratches
- Abnormal color
- Abnormal skin texture or temperature
- Hardened skin (orange peel texture)
- Other abnormalities as noted
Each of these conditions should be documented on the form to ensure proper follow-up care.
What should a CNA do if they notice an abnormality?
If a CNA observes any abnormal skin condition during the shower, they must report it to the charge nurse immediately. The charge nurse will then assess the situation and determine the appropriate intervention. It is essential for the CNA to document their findings on the form, including the specific location and nature of the abnormality, to facilitate further evaluation and care.
Is there a requirement for toenail care on the form?
Yes, the CNA Shower Sheets form includes a section to indicate whether the resident needs their toenails cut. This is an important aspect of personal care that can affect the resident's overall health and comfort. The CNA should check "Yes" or "No" based on their assessment during the shower.
How is the information on the form used after completion?
Once the CNA completes the form, it serves as a record of the skin assessment and any necessary interventions. The charge nurse reviews the form and may provide additional assessments or recommendations. If any issues are identified, the form is forwarded to the DON for further review. This process ensures that all skin abnormalities are addressed promptly and that the resident receives appropriate care.