Fill in a Valid Annual Physical Examination Form
Common PDF Forms
Dl 933 Form California Dmv - Ensure that you read and understand all certifications before signing.
Hurt Feelings Report - Having a formal process for reporting hurt feelings can bring relief to those suffering emotionally.
Understanding the nuances of a New York Residential Lease Agreement is essential for both landlords and tenants, as it provides clarity on key aspects such as rental terms, property maintenance, and legal responsibilities. For those seeking a comprehensive resource to help navigate this process, OnlineLawDocs.com offers valuable information that can assist in creating a well-structured agreement that promotes a harmonious rental experience.
Kink Form - Highlights a desire for aftercare following BDSM activities.
Misconceptions
Misconceptions about the Annual Physical Examination form can lead to confusion and incomplete submissions. Here are ten common misunderstandings, along with clarifications for each:
- All sections must be filled out for every appointment. Many believe that every section of the form is mandatory for all visits. In reality, only relevant sections need to be completed based on individual health needs.
- The form is only necessary for new patients. Some think that only new patients need to fill out this form. However, returning patients should also complete it to provide updated health information.
- Previous medical history is not important. It is a common misconception that past medical history does not need to be included. In fact, this information is crucial for understanding ongoing health issues and treatment plans.
- Only current medications need to be listed. People often believe that they should only list medications they are currently taking. However, it is important to include all medications, including those recently discontinued, as they can affect current treatment.
- Immunization records are optional. Some may think that providing immunization records is not necessary. In truth, these records are essential for assessing health risks and ensuring proper preventive care.
- All tests and screenings must be done annually. There is a belief that every test listed must be completed every year. However, the frequency of tests varies based on age, gender, and health conditions.
- Only serious health conditions need to be reported. Many individuals think they only need to mention significant health issues. It is beneficial to report all health conditions, even minor ones, as they may influence overall health assessments.
- Once the form is submitted, no further communication is needed. Some assume that submitting the form is the end of the process. In reality, follow-up may be necessary for clarifications or additional information.
- All patients will receive the same recommendations. There is a misconception that everyone will get the same advice based on the form. Recommendations are personalized based on the individual’s health status and needs.
- The physician will review the form only during the appointment. Some believe that the physician will only look at the form during the visit. In fact, many physicians review forms in advance to prepare for the appointment.
Understanding these misconceptions can help ensure that the Annual Physical Examination form is completed accurately and effectively, leading to better health outcomes.
Documents used along the form
When preparing for an annual physical examination, several other forms and documents may be required to ensure a comprehensive assessment of health. These documents can provide vital information about medical history, medications, and other health-related factors. Below is a list of commonly used forms that complement the Annual Physical Examination form.
- Medical History Form: This document collects detailed information about a patient's past illnesses, surgeries, and family medical history. It helps healthcare providers understand potential risk factors and tailor the examination accordingly.
- Medication List: A comprehensive list of all medications a patient is currently taking, including dosages and frequency. This helps prevent drug interactions and ensures that the physician has a complete picture of the patient's treatment regimen.
- Immunization Records: This document outlines the vaccinations a patient has received, including dates and types. Keeping this record up to date is crucial for assessing immunity and determining any necessary booster shots.
- Consent for Treatment Form: This form gives healthcare providers permission to perform examinations and procedures. It ensures that patients are informed about what to expect during their visit.
- Insurance Information Form: Patients must provide their insurance details to facilitate billing and coverage verification. This document helps streamline the administrative process during the visit.
- Patient Information Sheet: This form collects basic demographic information, including contact details and emergency contacts. It is essential for maintaining accurate records and ensuring effective communication.
- Advance Directive: This document outlines a patient’s wishes regarding medical treatment in case they become unable to communicate. It can guide healthcare providers in making decisions that align with the patient’s preferences.
- Referral Form: If a specialist consultation is necessary, this form provides the relevant information about the patient's condition and the reason for the referral. It ensures continuity of care and effective communication between providers.
- Motorcycle Bill of Sale Form: To ensure accurate documentation during a sale, refer to our comprehensive motorcycle bill of sale form guide for all necessary details.
- Release of Information Form: This document allows healthcare providers to share a patient's medical records with other parties, such as specialists or family members. It is crucial for coordinating care and maintaining transparency.
Each of these forms plays a significant role in the annual physical examination process. By ensuring that all necessary documents are completed and submitted, patients can help their healthcare providers deliver thorough and effective care. This preparation not only enhances the quality of the visit but also fosters a collaborative relationship between patients and their healthcare teams.
Steps to Filling Out Annual Physical Examination
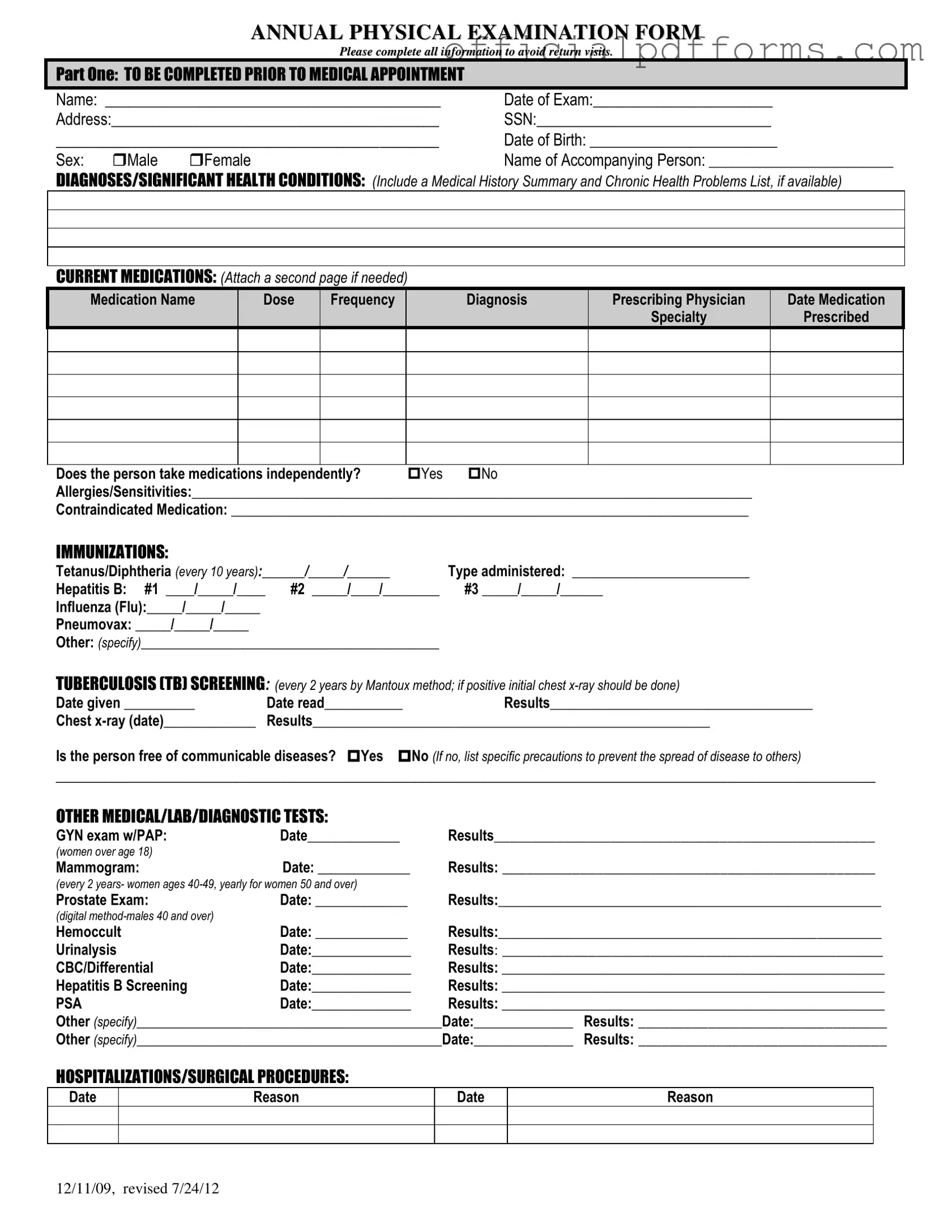
Completing the Annual Physical Examination form is an essential step in preparing for your medical appointment. Accurate information will help healthcare providers assess your health effectively. Follow these steps to ensure you fill out the form correctly.
- Start with Part One. Fill in your Name, Date of Exam, and Address.
- Provide your Social Security Number and Date of Birth.
- Select your Sex by marking either Male or Female.
- Write the name of the Accompanying Person if applicable.
- List any Diagnoses/Significant Health Conditions you have.
- Detail your Current Medications, including the name, dose, frequency, diagnosis, and prescribing physician. Attach a second page if necessary.
- Indicate whether you take medications independently by checking Yes or No.
- List any Allergies/Sensitivities and any Contraindicated Medications.
- Complete the Immunizations section with the dates and types of vaccines received.
- Fill in the Tuberculosis (TB) Screening details, including the date given and read, and the results.
- Provide information on other Medical/Lab/Diagnostic Tests you have undergone.
- Document any Hospitalizations/Surgical Procedures with dates and reasons.
- Move to Part Two. Record your Blood Pressure, Pulse, Respirations, Temperature, Height, and Weight.
- Evaluate each system listed and indicate if the findings are normal by checking Yes or No.
- Complete the Vision Screening and Hearing Screening sections.
- Provide any Additional Comments, including medication changes and recommendations for health maintenance.
- Note any limitations or restrictions for activities.
- Specify if you use adaptive equipment.
- Indicate any changes in health status from the previous year.
- Complete the physician’s information at the end of the form, including name, signature, address, and phone number.
Once the form is filled out, review it for accuracy. Bring it with you to your appointment to ensure a smooth and efficient visit.
Common mistakes
-
Incomplete Personal Information: Failing to fill out all sections of personal details, such as name, date of birth, and address, can lead to delays in processing and may require additional visits.
-
Neglecting Medical History: Omitting significant health conditions or previous diagnoses can hinder accurate assessments. This information is crucial for the physician to provide appropriate care.
-
Incorrect Medication Details: Not listing current medications accurately, including dosage and frequency, may result in dangerous interactions or ineffective treatment plans.
-
Missing Allergy Information: Failing to disclose allergies or sensitivities can pose serious health risks. It is essential to provide this information to ensure safe medical practices.
-
Ignoring Immunization Records: Not updating or accurately reporting immunization history may lead to unnecessary vaccinations or missed opportunities for preventive care.
Get Clarifications on Annual Physical Examination
What is the purpose of the Annual Physical Examination form?
The Annual Physical Examination form is designed to collect essential information about your health before your medical appointment. This helps your healthcare provider understand your medical history, current medications, and any significant health conditions you may have. By completing this form accurately, you can ensure that your physician has the necessary details to provide the best possible care during your visit.
What information do I need to provide in the form?
You'll need to fill out various sections of the form. Key areas include:
- Your personal information, such as name, address, and date of birth.
- A summary of your medical history and any chronic health problems.
- A list of current medications, including dosages and prescribing physicians.
- Details about any allergies or sensitivities.
- Immunization records and results from any recent medical tests.
Completing all sections thoroughly will help prevent any delays in your appointment.
Why is it important to list current medications?
Listing your current medications is crucial for several reasons. It allows your healthcare provider to assess potential interactions with any new treatments or medications they may prescribe. Additionally, knowing your medication history helps them understand your overall health better. If you are taking medications independently, it’s important to indicate that as well. This information can significantly impact your treatment plan.
What should I do if I have had recent hospitalizations or surgeries?
If you have had any recent hospitalizations or surgeries, it is important to provide that information on the form. You should include the dates and reasons for these medical events. This information helps your physician understand any changes in your health status and tailor your care accordingly. It can also alert them to any ongoing issues that may need to be addressed during your examination.
What happens if I don’t complete the form before my appointment?
Failing to complete the Annual Physical Examination form before your appointment may lead to delays. Your healthcare provider might not have all the necessary information to conduct a thorough examination, which could result in a need for follow-up visits. To avoid this, take the time to fill out the form completely and accurately prior to your visit. This will ensure a smoother and more efficient appointment.